80 y/f with complaints of shortness of breath and chest pain.
March 26, 2022
Treatment:
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 80 year old female came to casualty with complaints of shortness of breath and chest pain since 2pm (25/3/22)
History of presenting illness:
Patient was apparently asymptomatic 3years ago then she developed giddiness for which she diagnosed as hypertensive and used medications (Amlodipine 5mg, atenolol 50mg).
Pt has h/o fever on and off since 1yr which was relieved on medication.
Pt had generalised weakness since 2 days associated with sob which is grade II, then today at around 2pm, she developed shortness of breath which is grade IV(while at rest) for which she went to local hstpl and she used some medications and got symptoms subsided. At around 8pm again she developed SOB (grade IV) association with chest pain and came to casualty.
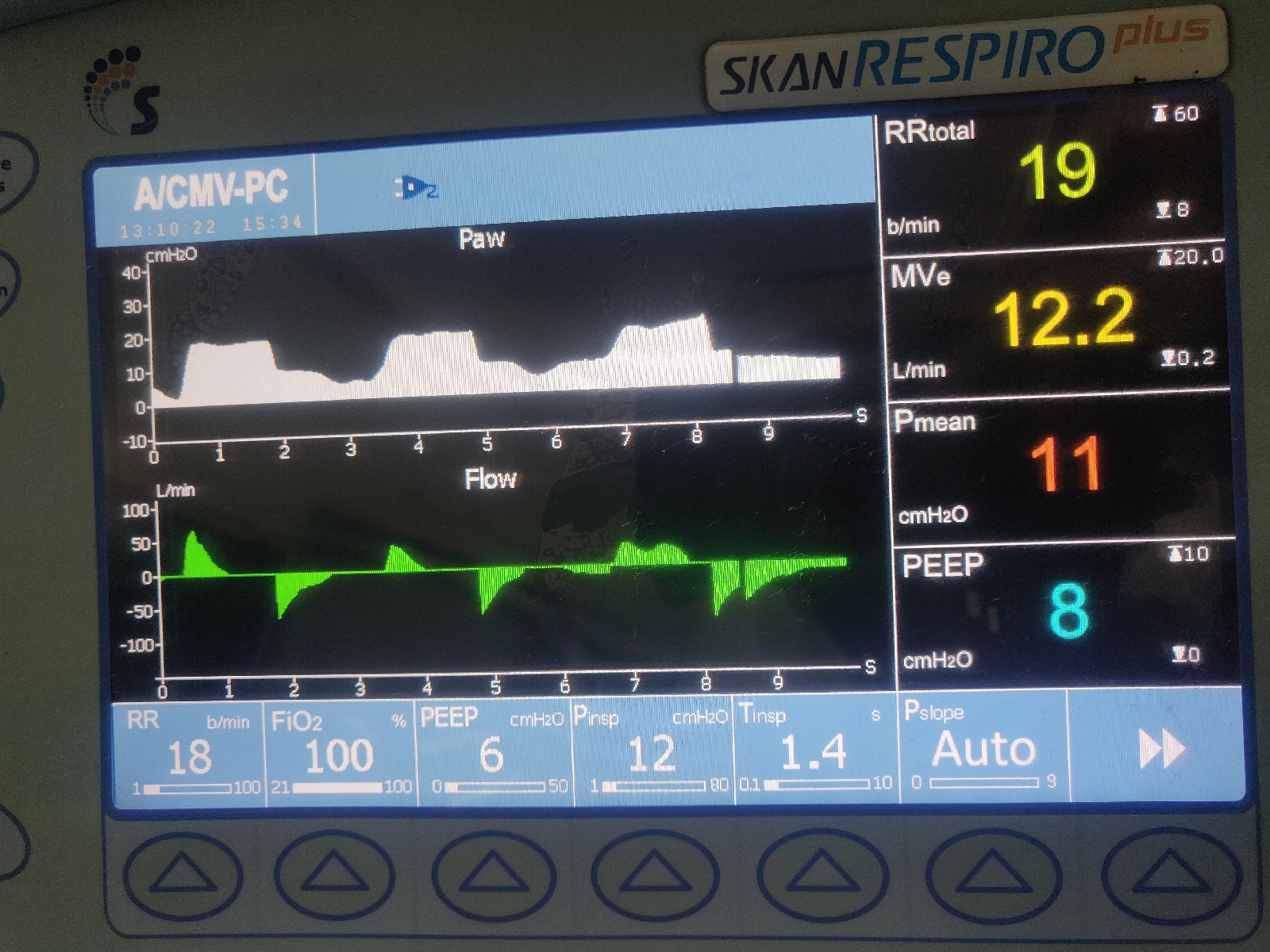
Patients spo2 was 40@Ra in the view patient was intubated at below settings.
After intubation patient got cardiac arrest pulse was week bp was non recordable. Then 3 cycles of cpr done along with adrenaline (1ml per each cycle of cpr).
Past history:
She was diagnosed with hypertensive 3 yrsback and was on medication.
Vitals on admission:
E1V1M1
PR: 90bpm
BP: 90/60 mm hg@norad6ml/hr, dobutamine 5ml/hr)
SpO2: 40% on RA
Cvs-s1s2 +
Rs-BAE+
P/a- soft
On examination,
Mild pallor present.
No icterus, cyanosis, clubbing, lymphadenopathy.
Post intubation ECG:
Today at 7am:
Serology - negative
Diagnosis:
? Unstable angina
?acute exacerbation of copd
Patient intubated 26/3/22 at 1:30am post cpr status 3 cycles.
1) inj.norad - 2amp in 46ml ns @6ml/hr.
2) inj dobutamine - 1amp in 45ml ns @5ml/hr
3) inj.Clexane - 60mg/sc/bd
4) tab.ecospirin 325/RT/stat
5) tab.clopidogrel 200mg/rt/stat
6) tab.atorvastatin 80mg/rt/stat
7) bp monitoring hrly
8)inj.NaHCo3 50mg/iv/stat
http://jadhavrajkumar.blogspot.com/2022/03/36-yf-with-complaints-of-shortness-of.html
NEW ADMISSION
26/3/22
ICU BED 1
S: PATIENT IS ON MAINTAINED MECHANICAL VENTILATION, NON SEDATED.
O:
Temperature: 98.6F
BP: 90/60 mmHg -NOR.AD 15ML/HR
-VASO 1ML/HR
-DOBU 5ML/HR
PR: 82 bpm
GRBS: 249mg/dl
Spo2: 95%@mech. ventilation
CVS: S1 S2 +,
RS: on ventilation
CNS: pt is drowsy and non responsive
P/A: soft
A:
CAD -ACS
? Unstable angina
?acute cardiogenic pulmonary edema.
S/p cpr - day 1 on mechanical ventilation
P:
1) inj.norad - 2amp in 46ml ns @6ml/hr.
2) inj dobutamine - 1amp in 45ml ns @5ml/hr
3) inj.Clexane - 60mg/sc/bd
4) tab.ecospirin 325/RT/stat
5) tab.clopidogrel 200mg/rt/stat
6) tab.atorvastatin 80mg/rt/stat
7) bp monitoring hrly
8)inj.NaHCo3 50mg/iv/stat
--------------------------------------------------------------
SOAP NOTES
27/3/22
ICU BED 1
S:
PATIENT IS ON MAINTAINED MECHANICAL VENTILATION, NON SEDATED.
O:
E1V1M1
BP-100/50 MMHG ON -NOR.AD 20ML/HR
-VASO 2ML/HR
-DOBU 5ML/HR
PR- 108/MIN
CVS-S1S2+
RS- BAE+
CNS- DOLLS EYE ABSENT
- B/L PUPILS CONSTRICTED,NON REACTING TO LIGHT CORNEAL, CONJUNCTIVAL REFLEX ABSENT.
P/A - SOFT
SPO2 - 95% ON FIO2 80%
TEMP- 103°F
PATIENT IS ON SIMV-V2
RR-14
FIO2- 80%
PEEP-6
VT-360
A:
CAD - ACS
? UNSTABLE ANGINA
WITH CARDIOGENIC PULMONARY EDEMA INTUBATED ON 26/3/2022 (POST CPR STATUS - 3 CYCLES).
P:
1) Rt feeds 100ml milk and 10ml water @4th hrly
2) inj.augmentin 1.2gm/iv/bd
3) inj.norad - 2amp in 50ml ns @20ml/hr.
4) inj dobutamine - 1amp in 50ml ns @5ml/hr
5) inj.vasopressin (1amp + 50ml NS) IV @2ml/hr
6) inj.heparin 5000IU /IV/QID
7) tab.ecospirin 150mg/RT/stat
8) tab.clopidogrel 200mg/rt/stat
9) tab.atorvastatin 40mg/rt/OD
10) Nebulisation with budecort and mucomist @8th hrly
11) vitals monitoring hrly
12) frequent post change every hrly
13) arterial and central line every 4th hrly
14) strict I/o charting












Comments
Post a Comment